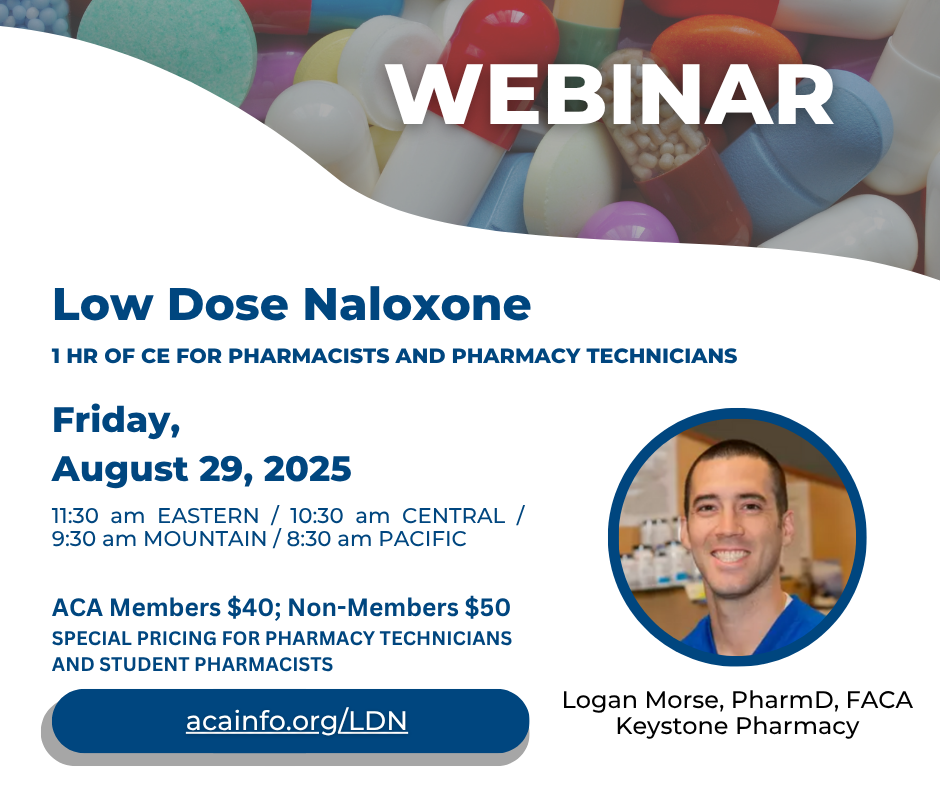
ACA WEBINAR: Low Dose Naloxone
Friday, August 29, 2025 | Time: 11:30 am Eastern / 10:30 am Central / 9:30 am Mountain / 8:30 am Pacific
Curious about the latest research and clinical uses of Low Dose Naloxone?
Registration isn’t open yet, and this activity is not yet accredited—but if you want to be the first to get updates and know when registration goes live, sign up for notifications today!
ACA Members $40; Non-Members $50
SPECIAL PRICING FOR PHARMACY TECHNICIANS AND STUDENT PHARMACISTS
Whether you’re interested in understanding the science behind Low Dose Naloxone or want to stay current on new clinical opportunities, this session offers timely insight for pharmacists and pharmacy technicians. Join the notification list below and be the first to know when registration opens!